In three major U.S. metropolitan areas, the mortality rate in nursing homes directly mirrored the rate of COVID-19 spread among the general population — to the point where the number of nursing home deaths in the city with the fewest total cases was not significantly higher than the same period in 2019.
That’s according to a new academic research letter from a team at Harvard, published this week in the Journal of the American Medical Association (JAMA).
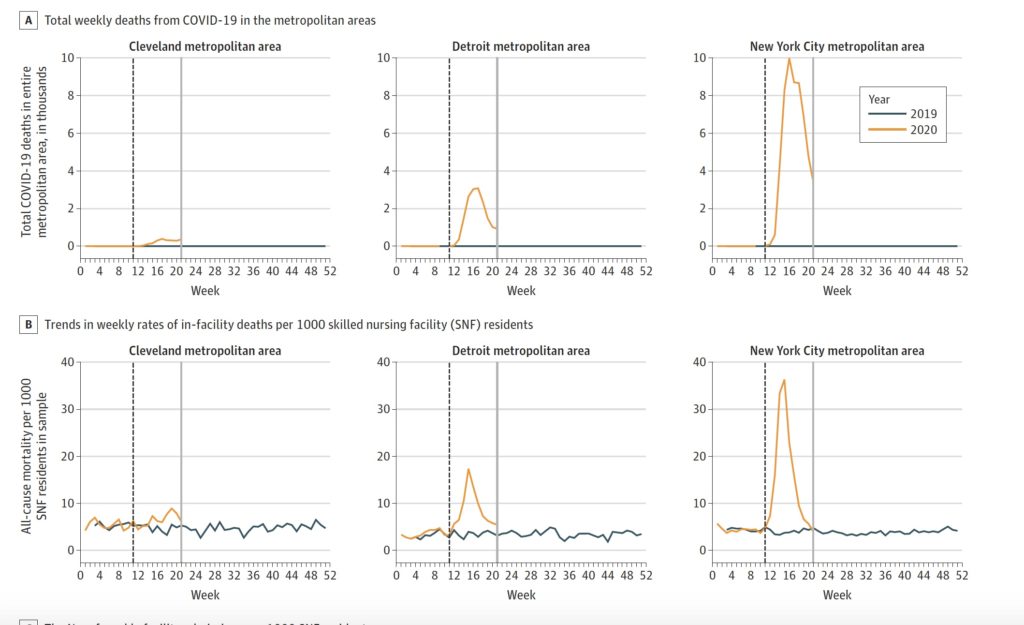
The researchers compare total death rates from a sample of skilled nursing facilities in the New York City, Detroit, and Cleveland metropolitan areas against the overall coronavirus impact on those regions.
“From March to May 2020, there was a spike in overall mortality among residents at SNFs in Detroit and New York City, which were two cities with substantial COVID-19 burden, and a lower increase in mortality in Cleveland, which was a city with fewer COVID-19 cases,” the researchers concluded. “Regardless of mortality, admissions and patient census decreased in all three cities.”
All three cities saw jumps in the death rate both generally and in nursing homes from 2019. In New York, for example, 13.8 out of every 1,000 nursing home residents died each week between March and May 2020, as compared with 4.1 out of 1,000 during the same period in 2019. Comparatively, the city saw a spike in the overall death rate between those timeframes of 3.7 to 36.3 per week.
In Cleveland, however, where the community outbreak was significantly more contained than in Detroit and New York, the mortality rate in SNFs increased only from 4.9 per 1,000 per week between March and May 2019 to 6.3 in 2020 — a difference that the researchers classified as “not statistically significant.”
The difference is striking when viewed in chart form below. The top row of charts illustrates the total weekly deaths among the general population in each city, while the bottom row shows the weekly death rate at skilled nursing facilities. The yellow lines track those figures in 2020, while the blue lines show the trends during the same months in 2019.
At the same time, all three cities experienced drops in skilled nursing facility admissions and census, in part likely due to the emergency cessation of all non-essential surgeries — which form a key pillar of demand for institutional post-acute care services.
“These results suggest that SNFs experienced substantial clinical challenges during the COVID-19 pandemic,” the researchers concluded. “Mortality increased quickly, raising concerns about the capacity of SNFs to respond to outbreaks. Compounding the challenge, decreased patient census may lead to reductions in revenue at a time when SNFs have the greatest need for additional resources to manage and prevent future outbreaks.”
Like all studies, this analysis has some caveats: The researchers did not consider the cause of each death, looking only at the raw numbers, and the sample of Cleveland facilities had a slightly higher average star rating than the total number of SNFs in the metro market. The analysis also only considered in-facility deaths; federal data on COVID-19 in nursing homes also includes deaths that occurred after a resident was transferred to a hospital.
In addition, the team emphasized that the three-city results can’t necessarily be extrapolated across all areas of the country. However, the letter contributes to a growing body of research indicating that the risk of outbreaks in nursing homes has many factors — including the racial and socioeconomic makeup of a community and facility size.
There have also been mixed conclusions on the correlation between star ratings and COVID-19 outbreaks, with some studies finding none and another seeing trends around RN staffing levels and overall star rating.
The most recent research letter was written by Michael Barnett and David Grabowski of Harvard, and Lissy Hu and Thomas Martin of CarePort Health, a Boston-based analytics and care coordination firm that aggregated data on SNF outcomes amid COVID-19.


