In March 2020, CMS announced a temporary freeze to measures and ratings across the Five-Star domain spectrum to allow nursing homes to prioritize resident and staff safety during the COVID-19 pandemic. In January 2021, CMS resumed calculating Nursing Home Compare data – though SNF Quality Rating Program (QRP) data remains frozen through 2022. Below, by comparing Nursing Home Compare data from March 2020 to July 2021, we examine SNF performance pre- and post-pandemic – and what may have occurred during COVID-19 to result in the following measures.
Staffing
One of the most interesting results we’ve examined in analyzing SNF performance throughout the course of the COVID-19 pandemic is related to staffing. Staffing ratings are comprised of registered nurse (RN) hours per resident day (RN HPRD) and total staffing hours (RN, LPN, CNA) per resident day (Total HPRD).
Both the RN HPRD and Total Staff HPRD measures have increased since the pandemic first began in the U.S. in March 2020:
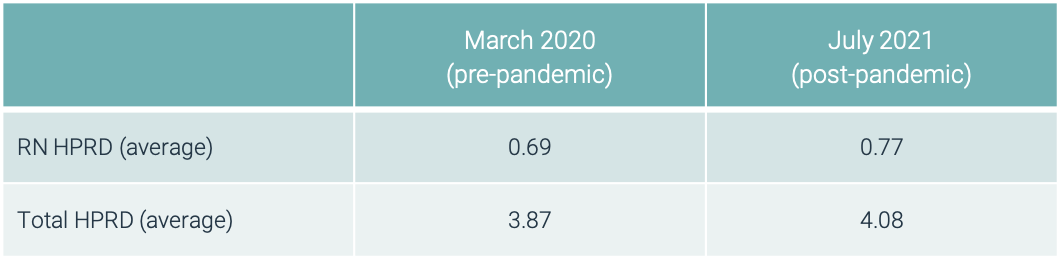
There is currently a narrative regarding widespread staffing shortages in post-acute care in the U.S. While it may be true that staff retention and hiring new employees at SNFs is challenging, RN HPRD and Total Staff HPRD have both increased due to continued low occupancy in SNFs (whereas we see a staffing shortage in home health due to increased demand).
As you might expect, patient acuity as defined by expected RN HPRD has risen over time – from 0.38 HPRD in March 2020 to 0.40 HPRD in July 2021. This increase tells us that while there are fewer patients in SNFs, their acuity is greater and therefore additional staff is required for their care.
Occupancy
Historically, SNF occupancy has hovered around 80%, on average. During the COVID-19 pandemic however, occupancy has plummeted. As of July 2021, average SNF occupancy sits at 70% – and SNF volume recovery remains slow as patients continue to opt for home-based care.
Five-Star Ratings
Until patients return to SNFs at pre-pandemic rates, staffing ratings appear to be better than they were pre-pandemic. These staffing ratings are, in reality, only driven by low SNF occupancy – but the increased staffing measures boost overall Five-Star averages. Overall Five-Star ratings have increased from 3.13 stars in March 2020 to 3.22 stars in July 2021.
Rehospitalizations and ED Visits
Two other components of the CMS Five-Star Quality Rating System are the 30-day rehospitalization rate and emergency department (ED) visits measure. The 30-day rehospitalization rate is the percentage of skilled patients who are discharged from a SNF and readmitted back to the hospital within 30 days, and the ED visits measure is percentage of Medicare Fee-for-Service (FFS) patients who have an ED visit within 30 days of entry or reentry to a SNF.
Another narrative we’ve heard is related to rehospitalizations, and that they may have spiked during the pandemic. Based on public data, however, that’s not necessarily the case.
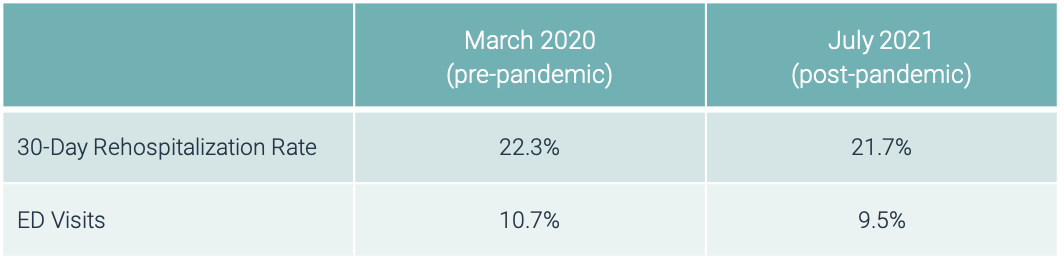
We actually see a slight decrease in both 30-day rehospitalization rates and ED visits over time. The measurement windows for those rates (below) encompass the majority of the pandemic:
- March 2020 data: Q3 2018 – Q2 2019
- July 2021 data: Q4 2019 – Q3 2020
2020 – and even throughout 2021 – have been an incredible test of resources and perseverance for SNFs across the U.S. As acute and post-acute care begin operating in a post-COVID-19 world, it’s important to remember that Five-Star ratings aren’t equipped to tell the whole story. For more visibility into SNF quality of care, we created the CarePort Quality Score, a ranking system that leverages real-time data – rather than relying on lagged data – to summarize the quality of care delivered by SNFs for short-stay patients.
Interested in learning more about the CarePort Quality Score? Contact us.