Preparing for What Comes Next: Where will COVID-19 Patients Recover?
Summary
Over 34,000 patients have been hospitalized for COVID-19 in New York City alone. As hospitalizations begin to flatten, the question facing New York will be: what comes next? One pressing and immediate issue to solve is where will COVID-19 patients who survive their hospitalization recover. Hospitalized COVID-19 patients often have underlying conditions and have severe COVID-19 disease requiring ICU stays and ventilators. After being in the hospital, COVID-19 patients will be de-conditioned and in need of rehabilitative care coming out of hospitals. Experts estimate that up to 30% of COVID-19 patients will need transitional care in facilities such as nursing homes.
Much of the attention to date has been on outbreaks among nursing homes where the elderly and disabled reside. Nursing homes serve a dual function in America; in addition to being long-term care facilities where the elderly and disabled reside, they are also “short-term” care settings where hospitals send their patients to recover after a severe illness. They are an essential part of the continuum of care, necessary to keep the entire system flowing. CarePort surveyed 8,942 nursing homes, which represent over 50% of nursing homes in the US, to better understand the impact of COVID-19 on the short-term rehabilitative component. Based on anecdotal reports, hospitals are facing challenges transitioning COVID-19 patients out of the hospital because understandably, nursing homes are reluctant to take in new patients. The nearly 9,000 nursing homes we surveyed over the last three weeks utilize CarePort to receive patient referrals from hospitals. Hospitals use CarePort to find short-term rehabilitative beds at nursing homes for patients to recover in. Our survey results show that fewer than 10% of nursing homes reported the ability to care for incoming COVID-19 patients. When hospitalized COVID-19 patients cannot leave the hospital because there is no place for them to recover, hospital capacity will be further exacerbated. In this report, we conduct a deep dive into New York to quantify the magnitude of this bottleneck. In New York City alone, there could potentially be a shortage of over 1,000 beds. In our next report, we plan on releasing the capacity of nursing homes across the country so that hospitals and public health officials can work together to prepare for what comes next: the COVID-19 nursing home bottleneck.
As part of a deep dive into New York, this report conducts an analysis of real-time data on 23,611 nursing home residents in New York, representing 20% of nursing homes in New York State. Much has been reported on the devastating effects of COVID-19 on nursing homes, where over 1.3 million Americans reside. Unfortunately, it has been tough to track COVID-19 in nursing homes given the lack of standardized reporting and challenges around testing. We hope our analysis in New York serves as a model for how public health officials can track COVID-19 in nursing homes in real-time until such time as testing is widely available.
Data Source
CarePort is a transitions of care platform used by 1,000 hospitals and 180,000 post-acute providers, including nursing homes, home health agencies, hospices, long-term acute rehabilitation hospitals, acute inpatient rehabilitation hospitals, dialysis facilities, and many more post-discharge settings of care. Real-time patient data from Allscripts, Epic, Cerner, Meditech as well as many skilled nursing and home health EHRs feed into the CarePort platform. CarePort has a national view of COVID-19 patients across hospitals of all sizes, disparate EHRs, and distributed across urban/suburban/rural locations in 43 states.
CarePort sees thousands of COVID-19 hospitalizations every day and tracks patients through their acute and then post-acute course of care. Given CarePort’s national footprint and visibility from the minute the patient enters the ED through their care journey post discharge, CarePort likely has one of the only cross-continuum views of COVID-19 patients that span care settings.
CarePort receives patient data from all hospital settings, including emergency rooms, inpatient units, and ICUs. Since CarePort tracks patients as they move through each of those settings, CarePort has a view into COVID-19 length of stay and outcomes (such as whether the patient required a ventilator, what procedures were performed, and whether the patient survived). Our data includes symptoms that patients present with as well as laboratory tests, so we can distinguish between suspected, exposed, and confirmed COVID-19 patients. This is important given the lack of testing and lag in testing in many areas. With this data, we can track a wider and likely more representative swath of COVID-19 patients (not just patients who were tested) and earlier in their care course. CarePort also captures patient demographic data (e.g. age, gender, ethnicity, insurance) as well as underlying conditions and comorbidities, so we can identify trends in who is being hospitalized and what patient characteristics correlates with outcomes.
Importantly, CarePort’s acute data is linked to post-acute data. Therefore, CarePort is able to present a holistic view of the COVID-19 patient. CarePort can report on cross-continuum outcomes that encompass both the hospital and post-hospital experience.
Given the breadth and depth of the CarePort data source, CarePort believes its observations can augment and complement the data that each hospital or nursing home has in its own EHR. The insights presented below are early and will likely evolve as CarePort sees thousands of new COVID-19 patients weekly. CarePort is releasing these early observations given the rapidly evolving nature of the pandemic and the need from hospitals and post-acute providers to have more data to help inform its COVID-19 response.
Part I: COVID-19 Survey Results from 8,942 Nursing Homes across the United States
Many COVID-19 patients will need to recover in nursing homes, yet few nursing homes are accepting COVID-19 patients, which could create bottlenecks on the backend for hospitals
Experts project that up to 30% of hospitalized COVID-19 patients will require short-term rehabilitative care in a nursing home (JAMA). Hospitals, in accordance with CMS regulations, are unable to discharge patients until a nursing home where the patient can convalesce is found.
CarePort surveyed nursing homes across the US to identify nursing homes able to care for recovering COVID-19 patients. CarePort surveyed 8,942 facilities in the last three weeks across 46 states. CarePort embedded this survey into its product, which is widely used by hospitals across the US to transition patients to nursing home and other recovery settings. CarePort estimates that on average 40% of patients across the US that transition to one of these post-discharge settings are facilitated via CarePort.
CarePort conducted this survey to assist its hospital clients in finding nursing homes that were willing and able to accept COVID-19 patients and ensure that COVID-19 patients could be safely transitioned to their next setting of care. This information is now included in a tool that hospitals can use to search for nursing homes. Having this information readily available can help reduce bottlenecks on the backend of a hospital stay.
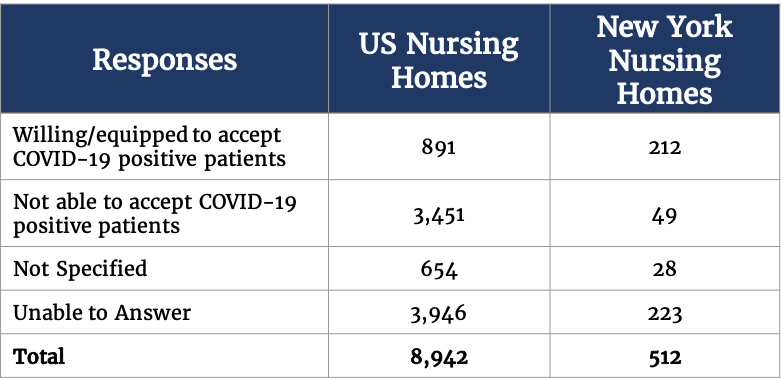
Only 10% of nursing homes nationally could affirm their ability to accept COVID-19 patients. 40% are not able to accept, and another 50% could not or would not specify.
Preparing for What Comes Next: Modeling Nursing Home Bed Needs for Recovering COVID-19 Patients Shows that New York Could Potentially Be Short 1,000+ Beds
In our survey of nursing homes in New York, 212 (41%) responded that they were able to accept COVID-19 patients; though 49% could not or would not specify. Notably, our survey was conducted after New York issued rules that require nursing homes take COVID-19 patients discharged from hospitals. However, although this requirement exists, there may be differences among nursing homes in their ability to care for COVID-19 patients. Nursing homes often lack critical supplies such as PPEs, isolation rooms and other specialized equipment needed to care for COVID-19 patients.
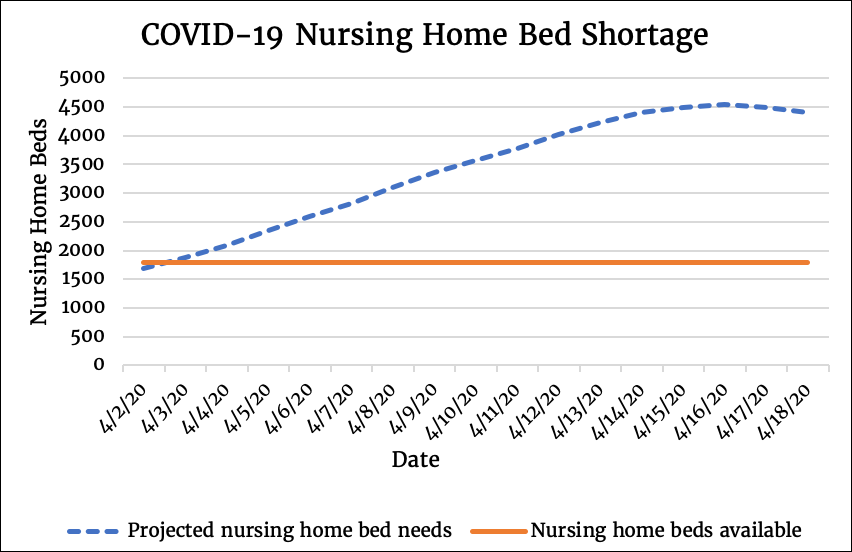
As of April 17, New York City has had 34K hospitalized cases for COVID-19. Below is a model for calculating nursing home bed needs for recovering COVID-19 patients:
Here are the critical inputs:
- Among hospitalized patients who survive (27,696 patients), 21% (5,816 patients) may need recovery beds in nursing homes in the coming weeks
- As of 3/15, CMS reported that there were 304 facilities within 25 miles of New York City with approximately 4,458 available certified SNF beds.
- Based on our survey results, 41% of nursing homes in New York City may be able to accept recovering COVID-19 patients, so potentially 1,828 beds would be available
- Not all beds will be able to be converted to COVID-19 convalescent beds as nursing homes are a mix of long-term residential and short-term rehabilitative beds. Assuming 80% could be converted, only 2,604 beds may truly be available for COVID-19 patients coming out of hospitals at any given time
The Details:
- In our analysis, we assumed only 21% of COVID-19 patients discharged from a hospital will require a SNF bed because the 30% estimate was based off Medicare patients, which traditionally have needed more rehabilitative care than younger patient populations. The 21% is based off our data which shows that 40% of hospitalizations are for patients over 60, and in that population, we assume 30% of the over 60 population will need nursing home care; the remaining 60% of hospitalizations are patients under 60, and in that population, we estimate that only 7% will require nursing home care. We are using the 7% estimate as that is the percentage of hospitalized COVID-19 patients currently being discharged to nursing homes in New York in practice based on CarePort data. (Of note, this percentage is unlikely to represent true demand for rehabilitative care and is more indicative of supply issues). The combination of the two gives a blended number of 21%. We recognize that this may be a conservative underestimate as anecdotally, we are hearing from our hospital partners that even many under 65-year-old patients are needing rehabilitative care. The hospitalized population are hospitalized because of severe COVID-19 disease no matter the age group.
- It is unlikely that 100% of the remaining capacity in nursing homes within a 25-mile radius of New York could be utilized for COVID-19 patients, so that is another area where this model may underestimate the shortfall
- The supply of nursing home beds may be increased due to the beds that are being vacated due to COVID-19 deaths. Potentially some of these residential beds could be converted to rehabilitative beds for recovering COVID-19 patients.
- Of note, there could also be patient preference issues at play which would alter demand for nursing homes. For example, since visitors are no longer allowed at nursing homes, patients may prefer to recuperate at home. However, unless the appropriate clinical and social support is arranged to be provided at home, these patients may be at high risk of hospital readmission. In the coming weeks, CarePort will be investigating whether there is a spike in readmission for COVID-19 patients who are discharged home.
Trouble on the horizon? Of 4,996 nursing facilities who responded nationally, only 10% affirmed their ability to accept COVID-19 patients coming from hospitals
Of the nearly 9K nursing homes surveyed, only 891 facilities indicated that they were able to care for new COVID-19 patients. This represents only 10% of facilities. Of note, the response rate varies state by state, and in areas where there are lower response rates, the respondents may not be a representative sample.
As COVID-19 surges occur throughout different areas of the US, it will be important to keep an eye on nursing home capacity. Nursing homes are an important part of the care continuum, and they are necessary to ensure that COVID-19 patients have the clinical support needed for their recovery. If these settings of care are unavailable, alternative care options will need to be identified to ensure a successful rehabilitation. Furthermore, without places for patients to recover, hospital capacity issues may be exacerbated at the worst possible moment.
By tracking post-acute capacity in relation to the surge in hospitalized patients, the state and federal government have a unique opportunity to get ahead of the virus. Hospitals on the ground need tools to help them determine which nursing homes can accept COVID-19 patients so as to ensure safe and effective transitions for COVID-19 patients. On a state and federal government-level, surge nursing homes may need to be constructed or converted to house COVID-19 patients in recovery to prevent bottlenecks from occurring at any point in our overall healthcare system.
Part II: An Analysis of 23K Nursing Home Residents in New York on 4/16
Nursing homes are transitional care settings for recovering patients coming out of hospitals, and they are also residential facilities for the elderly and disabled, who are especially vulnerable to severe COVID-19 disease given their age demographic and underlying conditions. Both aspects therefore must be considered when looking at the impact of COVID-19 on nursing homes. In this second part, we analyze symptoms of COVID-19 and the COVID-19 infection rate among 23K nursing home residents.
What is the real COVID-19 infection rate in nursing homes? Our data suggests 93% of nursing homes in New York could have COVID-19-positive patients
While the nursing home population’s high-risk nature has been recognized by the CDC, the CDC has yet to release any aggregated trends on COVID-19 in nursing homes. As of March 30, the CDC shared that there were 400 facilities with confirmed cases, while data from the states suggest that at least 2,300 nursing homes have COVID-19 cases. CarePort conducted a deep-dive analysis of 115 nursing home facilities in New York, representing 23,611 nursing home residents and 19% of nursing homes in the state.
As of April 16, more than 90% of New York City nursing homes in our sample were reporting any COVID-19 infections. Experts recognize that the infection rate is most likely higher than reported given the lack of testing. Based on our analysis of real-time symptoms and diagnosis data aggregated from nursing homes:
- 93% of nursing homes in New York City have COVID-19-positive patients.
- Furthermore, in 45% of New York City nursing homes, COVID-19 patients made up more than 10% of the population.
Of note, clusters of COVID-19 patients may be purposeful and not indicative of an outbreak in some cases. A common strategy for containment is to cohort COVID-19 patients. Some nursing homes have isolation rooms specifically designed for housing infectious patients. However, in areas where there are not enough isolation rooms for COVID-19 patients, nursing homes are converting entire buildings or wings to house COVID-19-only patients.
41% increase in nursing home patients reporting COVID-19-related symptoms (fever, cough, shortness of breath or pneumonia) in COVID-19 hot spots
Because of discrepancies around the availability of testing and the lag in testing data, CarePort also looked at COVID-19-related symptoms such as fever, cough, and shortness of breath as well as the COVID-19-related diagnosis of pneumonia.
At baseline, nursing home residents will have some level of fever, cough, shortness of breath symptoms as well as pneumonia. CarePort therefore looked at the relative increase each of these symptoms compared to the facility’s previous year’s prevalence rate as well as its rate compared to the national average. CarePort found that in New York, 58% of providers experienced a spike, as defined by a 1 standard deviation increase from previous year’s symptom prevalence and a current prevalence rate greater than 1 standard deviation in the national average, in one or more of the 4 COVID-19-related symptoms.
This sudden increase in patients reporting COVID-19-related symptoms over baseline is concerning when considering that the trajectory of COVID-19 transmission follows an exponential growth path. It points to a potential surge of COVID-19 in nursing homes – or a surge that has already happened and not yet confirmed due to lack of testing – in hot spot areas such as New York. Given how especially vulnerable nursing home residents are to COVID-19 infection, it is important to track the rise of COVID-19 in nursing homes. Having real-time data on COVID-19-related symptoms can give health systems and public health officials a leading indicator of COVID-19 infections, until testing is more widely available. At that point, nursing homes should be prioritized as care settings for wide-scale testing.