CarePort COVID-19 Insights: Mortality
Aggregated Observations from 6,479 Hospitalized COVID-19 Patients in the CarePort Network
April 2020 data from the CarePort Transitions of Care Hub
CarePort is a transitions of care platform used by 1,000 hospitals and 180,000 post-acute providers. Real-time patient data from Allscripts, Epic, Cerner and Meditech, as well as many skilled nursing and home health EHRs, feed into the CarePort platform. CarePort has a broad, national view of COVID-19 patients across hospitals of all sizes and distributed across urban, suburban and rural locations in 43 states.
CarePort manages thousands of COVID-19 hospitalizations every day and tracks patients through their acute and post-acute course of care. Given CarePort’s national footprint and visibility from the minute the patient presents at the emergency department through their care journey post-discharge, CarePort has a comprehensive view of COVID-19 hospitalizations and post-discharge needs.
CarePort receives patient data from all hospital settings, including emergency rooms, inpatient units and ICUs. Because CarePort tracks patients as they move through each of those settings, CarePort has a view into COVID-19 length of stay and outcomes – such as whether the patient required a ventilator, what procedures were performed and whether the patient survived. Our data includes symptoms that patients present with, as well as laboratory tests, so we can distinguish between suspected, exposed and confirmed COVID-19 patients. This is important given the lack of testing and lag in testing in many areas. With this data, we can track a wider and likely more representative swath of COVID-19 patients – not just patients who were tested – and earlier in their care course. CarePort also captures patient demographic data (e.g. age, gender, ethnicity, insurance) as well as underlying conditions and comorbidities, so we can identify trends in who is being hospitalized and what patient characteristics correlate with outcomes.
Importantly, CarePort’s acute data is linked to post-acute data. Therefore, CarePort is able to present a holistic view of the COVID-19 patient. CarePort can report on cross-continuum outcomes that encompass both the hospital and post-hospital (nursing home and home health) experience.
Given the breadth of the CarePort data source, we believe our observations can augment and complement the depth of data that each hospital has in its own EHR. The insights presented below are preliminary and will likely evolve as CarePort sees thousands of new COVID-19 patients weekly. CarePort is releasing these early observations given the rapidly evolving nature of the pandemic, and hospitals’ need for more data to help inform their COVID-19 response.
Below are preliminary observations from 6,479 hospital stays of patients admitted after March 1, 2020. For context, the CDC report on hospitalization-related outcomes released on Wednesday, April 8, 2020 included 1,482 hospitalizations. This report is also significant in that all 6,479 stays are concluded and have known outcomes.
Male patients are 1.3 times more likely to die during a hospital stay even after controlling for age and the most common underlying conditions
Several reports in China, Italy and the US have identified that the gender breakdown of patients with severe outcomes skews towards male. However, it is not well understood whether male patients have worse outcomes because they are disproportionately older or have more underlying comorbidities. Our data, for the first time, shows that men are 1.3 times more likely to die during a hospitalization, even after controlling for age and common underlying conditions. These results may be potentially confounded, as we did not control for all underlying conditions. However, we did take into account the most prevalent chronic conditions in the US, including chronic kidney disease, cerebrovascular disease, congestive heart failure, obesity, diabetes, COPD and hypertension. Interestingly, the predilection of males for severe disease is also seen in the pediatric data that the CDC recently reported on April 10, 2020. One would not expect the pediatric population to have differences in chronic conditions between male and female patients. If male patients do indeed fare worse than female patients, this may have implications for clinical triage, treatment and potentially vaccine efficacy.
Hospitalized COVID-19 patients with multiple underlying medical conditions are at high risk for mortality
A 75-year-old with no underlying conditions has a mortality rate of 16-19% when hospitalized with COVID-19. Though a decade younger, a 65-year-old with hypertension, diabetes, chronic kidney disease and/or obesity has a similar mortality rate as the 75-year-old with no underlying conditions. This example illustrates the differential impact of underlying health conditions on the risk of severe disease. As consistent with prior reports, we observed that trends in mortality varied based on the number of underlying health conditions. Specifically, CarePort examined the impact of common chronic conditions such as heart failure, diabetes, cerebrovascular disease, COPD, hypertension, chronic kidney disease and obesity.
CarePort’s observations below give an early indication of risk after adjusting for age (Table 2). It is important to adjust for age as older patients may be more likely to have chronic conditions. Without controlling for age, it is unclear whether age or the underlying condition drives a higher risk of mortality – but when adjusting for age, we can more clearly isolate the impact of an underlying condition. For example, patients with chronic kidney disease are 2.5 times more likely to die during a COVID-19 hospitalization after controlling for age.
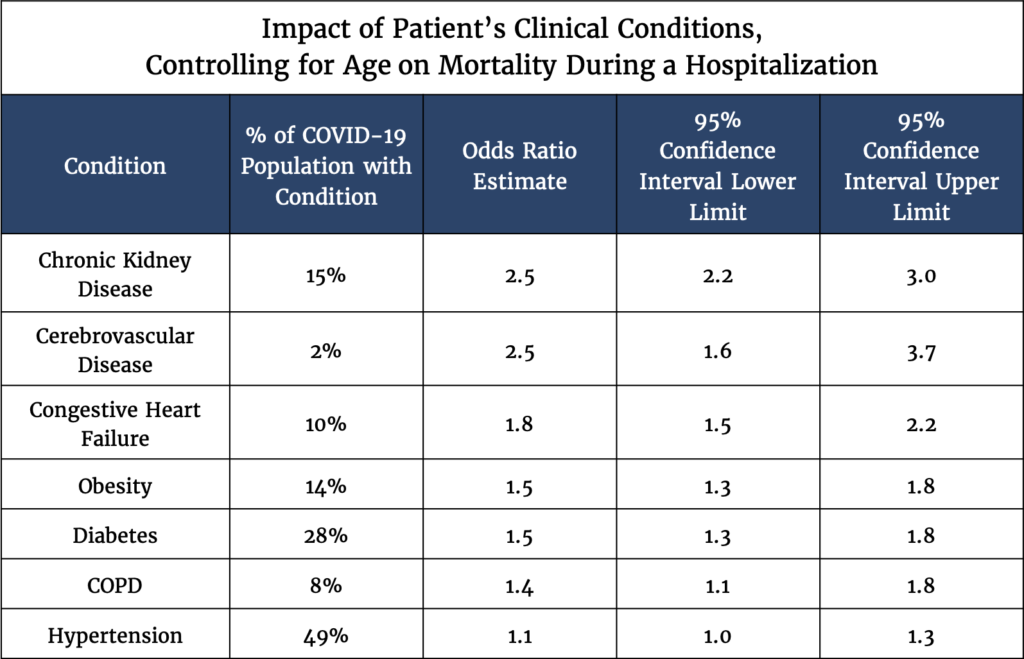
Table 1
Though these observations are similar to the April 8 CDC report, they do not take into account the severity of these underlying conditions, which can vary widely across patients. Furthermore, this analysis examines clinical conditions on their own, when in reality many of these symptoms track together; this is important because of interactions between underlying conditions. For example, a patient with chronic kidney disease may be more likely to have acute kidney injury, so the odds ratio may be overstating the impact of chronic kidney disease. It is also unclear in our data why hypertension does not seem to convey higher risk.
Acute kidney injury in COVID-19 patients is associated with poor outcomes across all age groups
In the context of COVID-19, our data signal that acute kidney injury increases the risk of mortality. For example, a hospitalized 85-year-old with no underlying conditions has a mortality rate of 22-27%. If that same 85-year-old is hospitalized with acute kidney injury, his mortality rate nearly doubles to 39-49%.
When the kidney is injured over a few hours or days, the medical term is “acute kidney injury”. The kidney is often an early casualty of other disease processes occurring in the body. Clinicians routinely measure kidney function with a blood test upon admission to the hospital, and the presence or absence of acute kidney injury is a prognostic indicator commonly used in multiple models of mortality.
1 in 10 middle-aged COVID-19 patients do not survive their hospital stay
Across CarePort hospitals, 1,123 COVID-19 patients have died during hospitalization. The mortality rate was highest among those aged 85 and older, with more than 40% of hospitalized patients dying during their hospital stay (Table 2). However, even among the middle-aged population (ages 45-64), the risk of mortality during a hospital stay is significant, with a 9% mortality rate in the 45-54 population and a 13% mortality rate in the 55-64 patient population.
Notably, these observations are from a patient population that is already hospitalized and at baseline, these patients are already likely showing severe disease requiring hospitalization. Therefore, these data cannot be generalized to all middle-aged patients who develop COVID-19 as many do not require hospitalization.
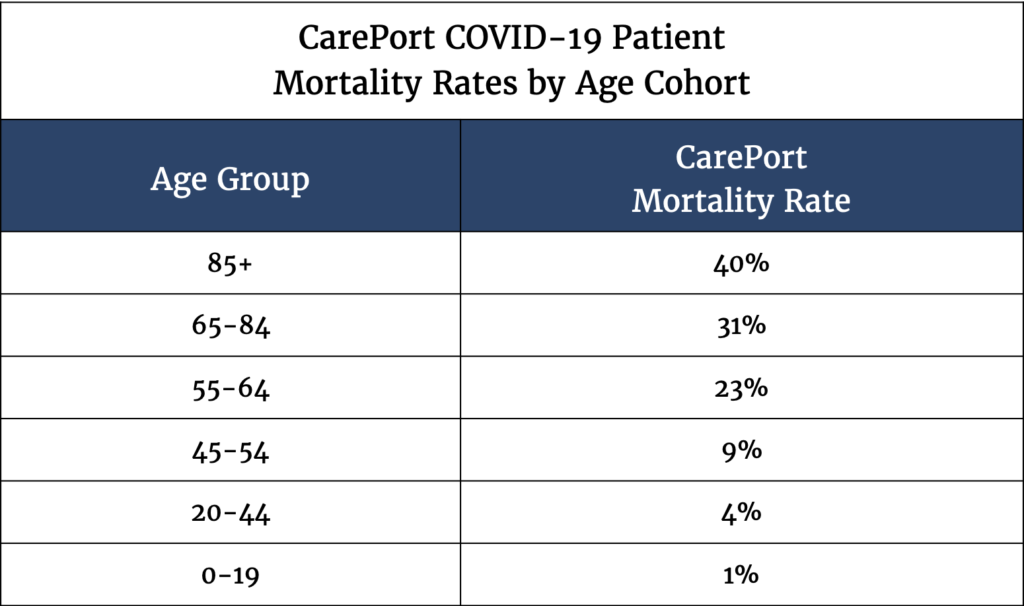
Table 2
Patients under 65 comprise 57% of hospitalizations for COVID-19
CarePort data (Table 3) shows that a significant portion of COVID-19 hospitalizations (57%) are for patients under the age of 65, which aligns with CDC data (55%). The average age of a patient hospitalized with COVID-19 is 59.6 years old. The experience of our hospitals further confirms that COVID-19 is a medical condition that impacts a broad swath of the population, not just seniors.
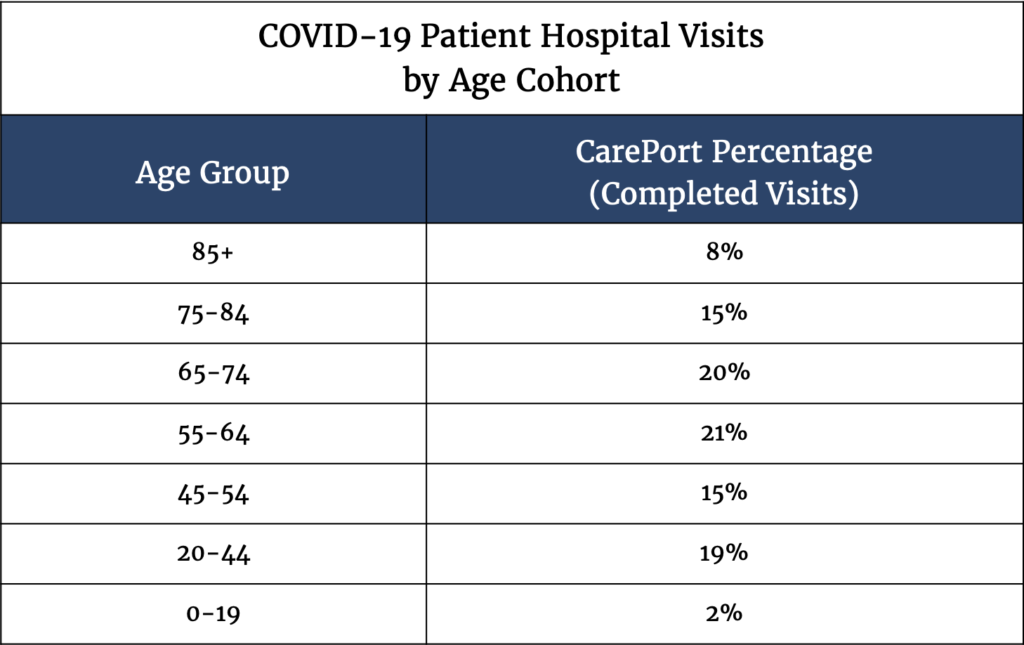
Table 3
Looking Ahead
The observations represent a uniquely broad and deep view of hospitalized COVID-19 patients across the US. Given the richness of CarePort data, many subsequent analyses are possible and are actively being pursued. For example, CarePort is investigating the association of comorbidities with hospital length of stay and ventilator use to help further refine models of resource utilization and assist hospitals with strategic planning. On the clinical side, the incorporation of clinical laboratory data, such as blood tests that hospitals routinely take upon admission, could further help predict risk in COVID-19 patients. CarePort’s linked acute and post-acute data can also help hospitals prepare for what comes next – the post-acute surge. Many COVID-19 patients will need nursing home or home health care, and CarePort can help identify where there is capacity on the post-acute side so that the discharge of COVID-19 patients does not become a bottleneck for hospitals. Additionally, since CarePort follows patients post-discharge, CarePort has the ability to track readmissions of COVID-19 patients and other downstream outcomes. CarePort expects to have ongoing, additional insights.
Given the rapidly evolving nature of this pandemic, CarePort sought to release this data early for the benefit of hospitals that are trying to manage the virus. As such, these early observations should be viewed as signals that may be directionally correct. There are many limitations associated with preliminary data. For example, one important limitation of this analysis is that ongoing stays (i.e. patients who were admitted in March who remain hospitalized) were excluded. As such, we do not yet know the impact of patients with potentially long lengths of stay and further follow-up time is required for these active stays. These data are raw and will require much further analysis. To that end, CarePort seeks academic partners who may be interested in collaborating in subsequent analysis and validation. To learn more, please email careport@careporthealth.com.
About CarePort
CarePort is an Allscripts Company that provides a care coordination network used by 1,000 hospitals and 180,000 post-acute providers in 43 states. We share this data in the hopes of improving the lives of all Americans, consistent with Allscripts’ mission of partnering with clients to build open, connected communities of care, and our belief that when such conditions are created, innovation flourishes. To subscribe to additional insights, please visit www.covidtoc.com.