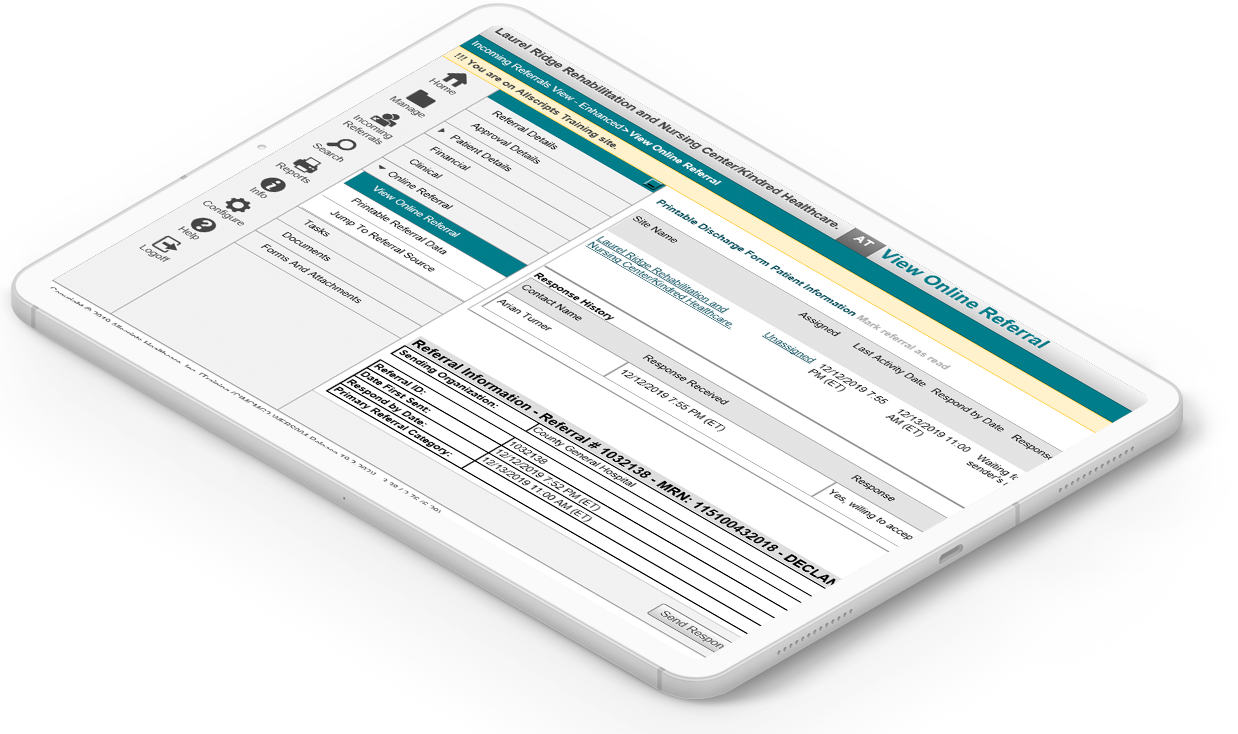
CarePort Referral Management
Receive, respond and review all patient referral activity in a single electronic system.
Click below to view CarePort (AllScripts/ECIN) referrals or to learn more about getting started.

2k
hospitals
130
K
in-network Post-acute providers
52
M
annual Referrals
8
min
electronic referral response time
Receive and respond electronically to patient referrals in a single system
A total solution for referral automation and post-acute discharge planning
- Automatically receive and respond to referrals, and discharge patients to another level of care
- Receive alerts of incoming referrals to your computer or mobile device to minimize missed referral opportunities
- Customize worklists that fit your intake process and enter referrals from non-electronic sources
- Increase visibility to referral sources in the CarePort database
- Admit patients right from the referral work list, eliminating manual entry and helping to retain key data
Improve patient engagement and satisfaction with a streamlined care transition process
- Select the right care provider for your patient’s next level of care needs
- Generate comprehensive reports
- Integrate with post-acute EHRs to eliminate the re-keying of referral information
- Send post-acute authorization requests to payers and track responses
Flexible workflow for organizations of all kinds
- Streamline the authorization process between payers and providers to help ensure members go to in-network organizations
- Connect community-based services and organizations with referring sources such as hospitals or care centers to address patients' social determinants of health


Overview : Press Release
CarePort Health Survey of Nearly 9K Nursing Homes Across the Country Projects Healthcare Bottlenecks, Bed Shortages
CarePort today released a new report: Preparing for What Comes Next: Where Will COVID-19 Patients Recover? The report leverages real-time patient data from CarePort’s transitions-of-care platform, as well as a survey of nearly 9,000 nursing homes across the United States.
Next : read the press release hereRequest a Demo
See how CarePort’s solutions would work in your organization.
