In our first virtual care coordination summit, “COVID-19 in Detroit,” we learned how Henry Ford Health System, Advantage Living Centers and Health Alliance Plan (HAP) worked together to successfully coordinate cross-continuum patient care during Detroit’s COVID-19 surge. We explored the key themes contributing to the three stakeholders’ success – pivoting quickly, increasing communication, and collaborating across the continuum – in a recent blog post.
Below, we summarize HAP’s experience during the COVID-19 pandemic – including their care management processes, partnering with Henry Ford and CarePort, and lessons learned as they continue to navigate these complex times. Joining us from HAP during our virtual care coordination summit were Dr. Peter Watson, Vice President, Care Management, Quality and Outcomes; Catherine Smith, Director, Utilization Management, and (Interim) Director, Case Management and Government Programs; and Matthew Tebbe, Manager, Demand Management and Capacity Planning.
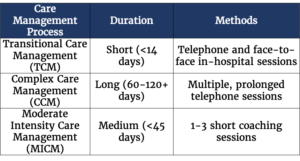
HAP Care Management Processes
During the COVID-19 surge in Detroit, HAP expanded initiatives (outlined below) typically only utilized for specific member populations. These supplemental benefits, typically reserved for Medicare Advantage members, were extended to include all lines of business and included calling at-risk or COVID-19-positive members that might benefit from meal delivery, as well as checking in on members at-risk for loneliness or depression and offering behavioral health services and meal delivery.
HAP moved swiftly to ensure members’ access to care wasn’t impacted during an uncertain time. When Michigan declared a state of emergency, HAP immediately ceased all authorization requirements for SNF placement. This measure automatically provided authorization for COVID-19-related illnesses, helping facilitate the necessary care for inpatient members. HAP also relaxed outpatient authorization requirements for anything pertaining to COVID-19, waived appeal timelines, allowed early refills on medications, promoted pharmacy home delivery at no additional cost to members, and offered free access to COVID-19-related behavioral health resources.
To ensure patients received the necessary treatment, HAP also waived cost share for COVID-19 testing and treatment, and increased the amount of care provided virtually. HAP’s telehealth visits, averaging 1,000 per month pre-pandemic, spiked to nearly 86,000 at the peak of COVID-19. Because the COVID-19 peak in Detroit has passed, telehealth visits have declined, but are still significantly higher than they were prior to COVID-19 – and HAP hopes to continue to experience growth in this area. Since the COVID-19 outbreak began in Michigan, HAP has made between 11,000 to 12,000 telephonic reach outs to its members.
Partnering with Henry Ford and CarePort
Not only did HAP assist members by increasing access to care, but it also helped its acute partner, Henry Ford, when they faced significant referral and discharge process complexities. When COVID-19 reached Detroit, SNFs began denying COVID-19-postive patients, which made it increasingly difficult for Henry Ford’s case managers and discharge planners to secure SNF placement and discharge patients to a lower level of care. HAP worked closely with Henry Ford during this time to remove barriers to care and to simplify SNF placement for its acute partner. Through daily huddles and operational calls with Henry Ford, HAP could better understand where there were gaps in care, and how they could help streamline transitions of care.
HAP utilized ICD-10 codes from CarePort for real-time potential COVID-19 hospital admissions – rather than having to wait for claims data, which was even more delayed than normal as hospitals focused on their patient surges. HAP and CarePort worked together to develop a reporting structure sharing COVID-19 test results, which was sent to HAP on a daily basis and soon thereafter incorporated into the CarePort platform. HAP built dashboards around CarePort’s COVID-19 data, and now leverages this real-time data to predict future COVID-19 outbreaks, and to help predict business and financial impacts.
Lessons Learned and Looking Ahead
Through this experience, HAP has learned the critical importance of increased communication – through its relationship with Henry Ford, as well as real-time data and notifications – provided by the CarePort platform. Leveraging data from these two sources, HAP can better ensure that, as a health plan, they are doing their part to facilitate cross-continuum care.
Looking ahead, HAP is already preparing a response mechanism for the fall, and will leverage patterns within CarePort data to prepare for a potential overlap in COVID-19 and influenza surges to ensure it can best support its partners. HAP will utilize CarePort as a more effective early warning tool, and will monitor aggregated symptoms and admissions trends to quickly identify hotpots in the area using the platform’s real-time data.
CarePort data will also inform ongoing efforts to improve social determinant interventions. HAP has expanded and continues to explore nontraditional ways to support the medical needs of the community. As a payer, HAP seeks to redirect premium to those areas that can address social determinants, and keep people safe in their homes. These efforts may help offset hospital surge needs while still ensuring members receive the appropriate level of care.
Watch the full-length recording of our live case study, and learn more about Henry Ford’s experience in our recent blog post. Stay tuned for an upcoming blog post that shares how Advantage Living Centers managed the COVID-19 surge in Detroit.